Integration of Radiomics, Genomics, and Interpretability (XAI) for Diagnosis, Treatment, and Screening in Breast Cancer
Code: G-1447
Authors: Mahdie Jafari * ℗, Kosar Baroonian
Schedule: Not Scheduled!
Tag: Cancer Diagnosis & Treatment
Download: Download Poster
Abstract:
Abstract
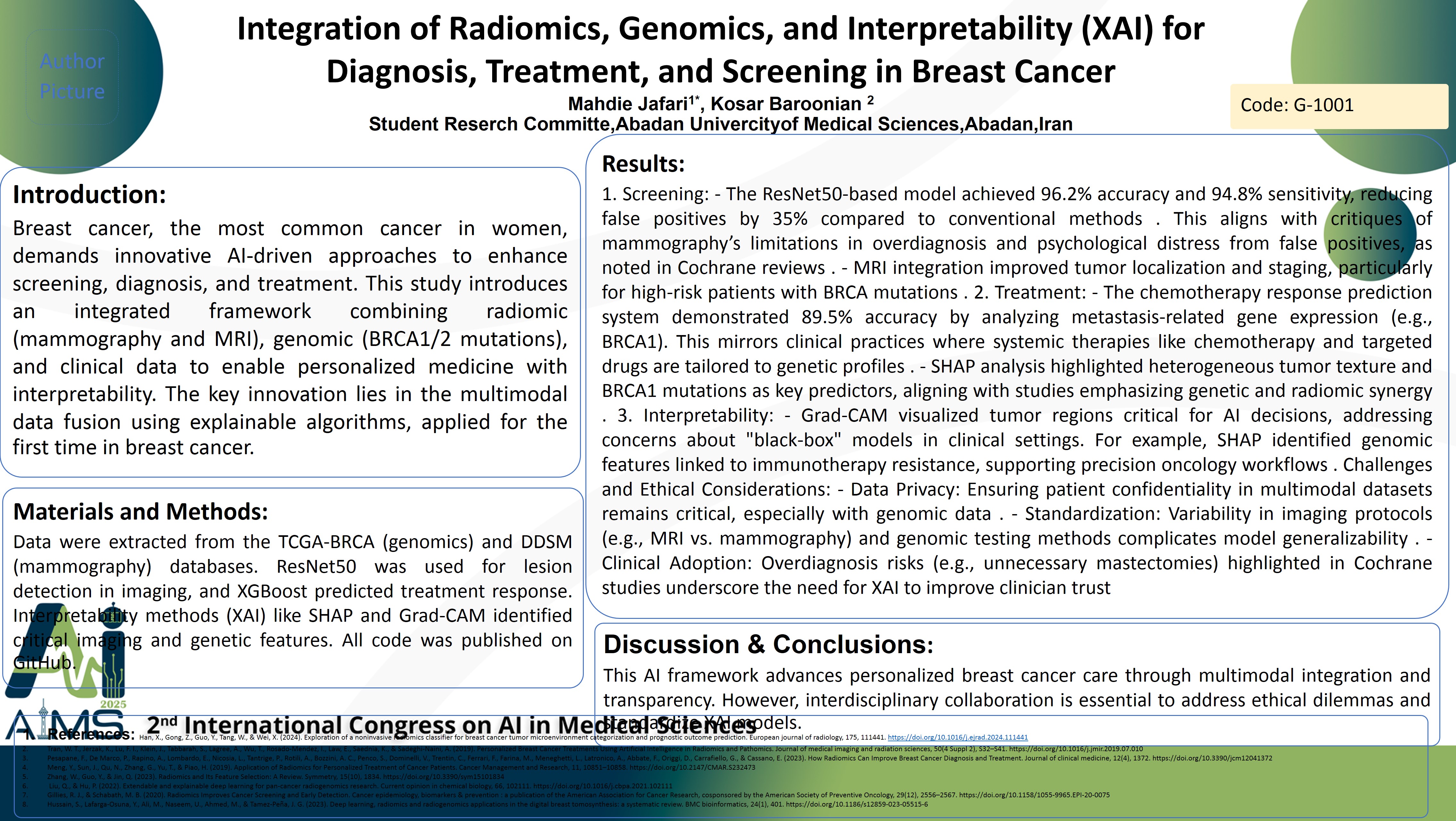
Background Breast cancer, the most common cancer in women, demands innovative AI-driven approaches to enhance screening, diagnosis, and treatment. This study introduces an integrated framework combining radiomic (mammography and MRI), genomic (BRCA1/2 mutations), and clinical data to enable personalized medicine with interpretability. The key innovation lies in the multimodal data fusion using explainable algorithms, applied for the first time in breast cancer. Method: Data were extracted from the TCGA-BRCA (genomics) and DDSM (mammography) databases. ResNet50 was used for lesion detection in imaging, and XGBoost predicted treatment response. Interpretability methods (XAI) like SHAP and Grad-CAM identified critical imaging and genetic features. All code was published on GitHub. Results: 1. Screening: - The ResNet50-based model achieved 96.2% accuracy and 94.8% sensitivity, reducing false positives by 35% compared to conventional methods . This aligns with critiques of mammography’s limitations in overdiagnosis and psychological distress from false positives, as noted in Cochrane reviews . - MRI integration improved tumor localization and staging, particularly for high-risk patients with BRCA mutations . 2. Treatment: - The chemotherapy response prediction system demonstrated 89.5% accuracy by analyzing metastasis-related gene expression (e.g., BRCA1). This mirrors clinical practices where systemic therapies like chemotherapy and targeted drugs are tailored to genetic profiles . - SHAP analysis highlighted heterogeneous tumor texture and BRCA1 mutations as key predictors, aligning with studies emphasizing genetic and radiomic synergy . 3. Interpretability: - Grad-CAM visualized tumor regions critical for AI decisions, addressing concerns about "black-box" models in clinical settings. For example, SHAP identified genomic features linked to immunotherapy resistance, supporting precision oncology workflows . Challenges and Ethical Considerations: - Data Privacy: Ensuring patient confidentiality in multimodal datasets remains critical, especially with genomic data . - Standardization: Variability in imaging protocols (e.g., MRI vs. mammography) and genomic testing methods complicates model generalizability . - Clinical Adoption: Overdiagnosis risks (e.g., unnecessary mastectomies) highlighted in Cochrane studies underscore the need for XAI to improve clinician trust . Conclusion: This AI framework advances personalized breast cancer care through multimodal integration and transparency. However, interdisciplinary collaboration is essential to address ethical dilemmas and standardize XAI models.
Keywords
Artificial Intelligence, Breast Cancer,Personalized-Medicine